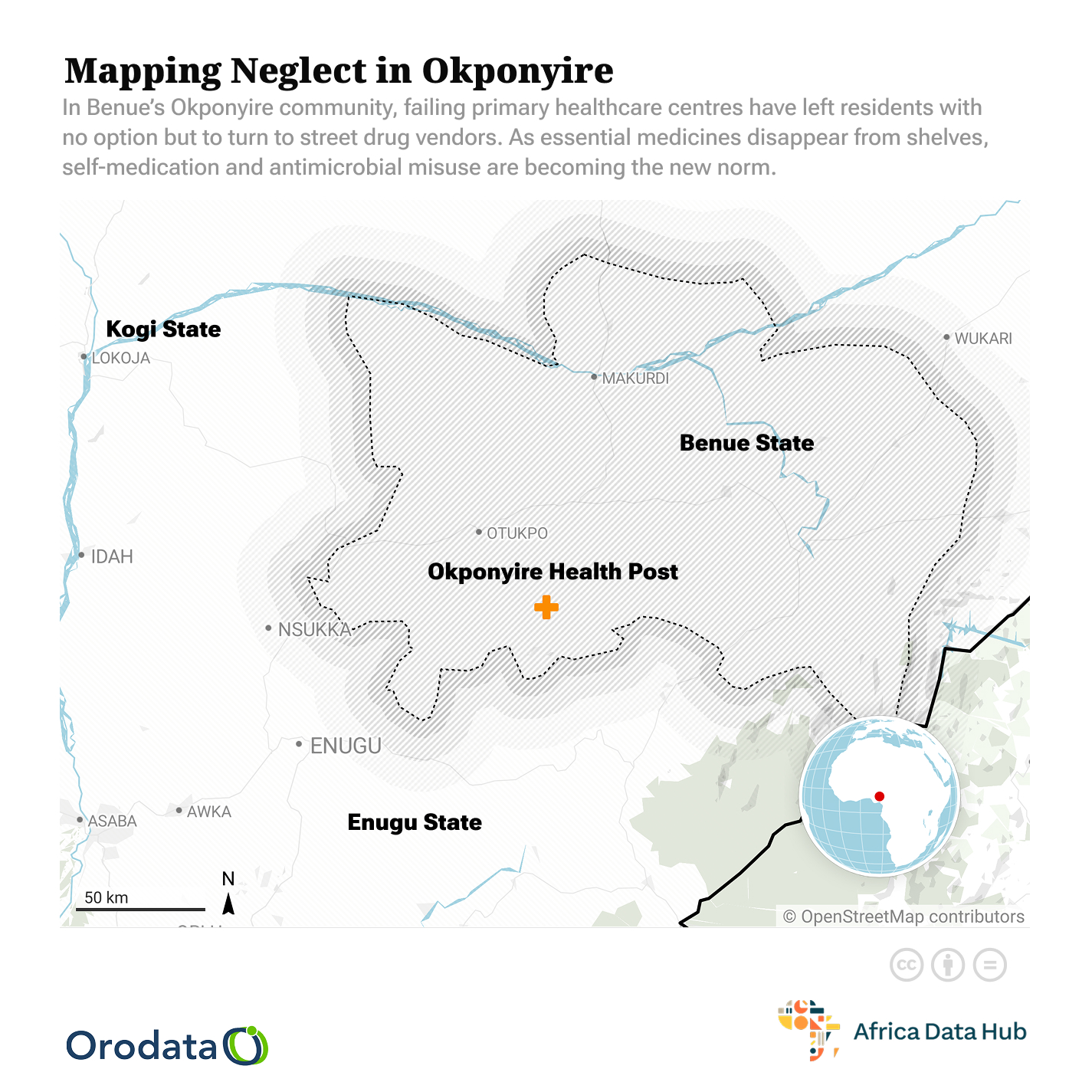
The dire state of primary healthcare centres – characterised by chronic drug shortages and inadequate infrastructure – is forcing communities into a dangerous reliance on self-medication.
By: David Arome
On 30th November, 2023, Inori Elijah, residing in the Otokwe community, Obi local government area (LGA), Benue State, had a near-death experience of malaria and typhoid fever co-infection that almost took her life. With the feverish symptoms, she still struggles to harvest her beans from the long-trekked distance farm. Just a few minutes’ walk from the farm, she fell on the footpath with the harvested beans. Lying helpless until a co-farmer on a bike picked her up.
One of the PHCs with Drug shortages: Photo Credit: Otokwe Primary Health Centre, captured by David Arome
She was rushed to the nearby health outpost for treatment but found the health facility closed. While waiting, a call was put through to the officer in charge (OIC) to come over to treat her.
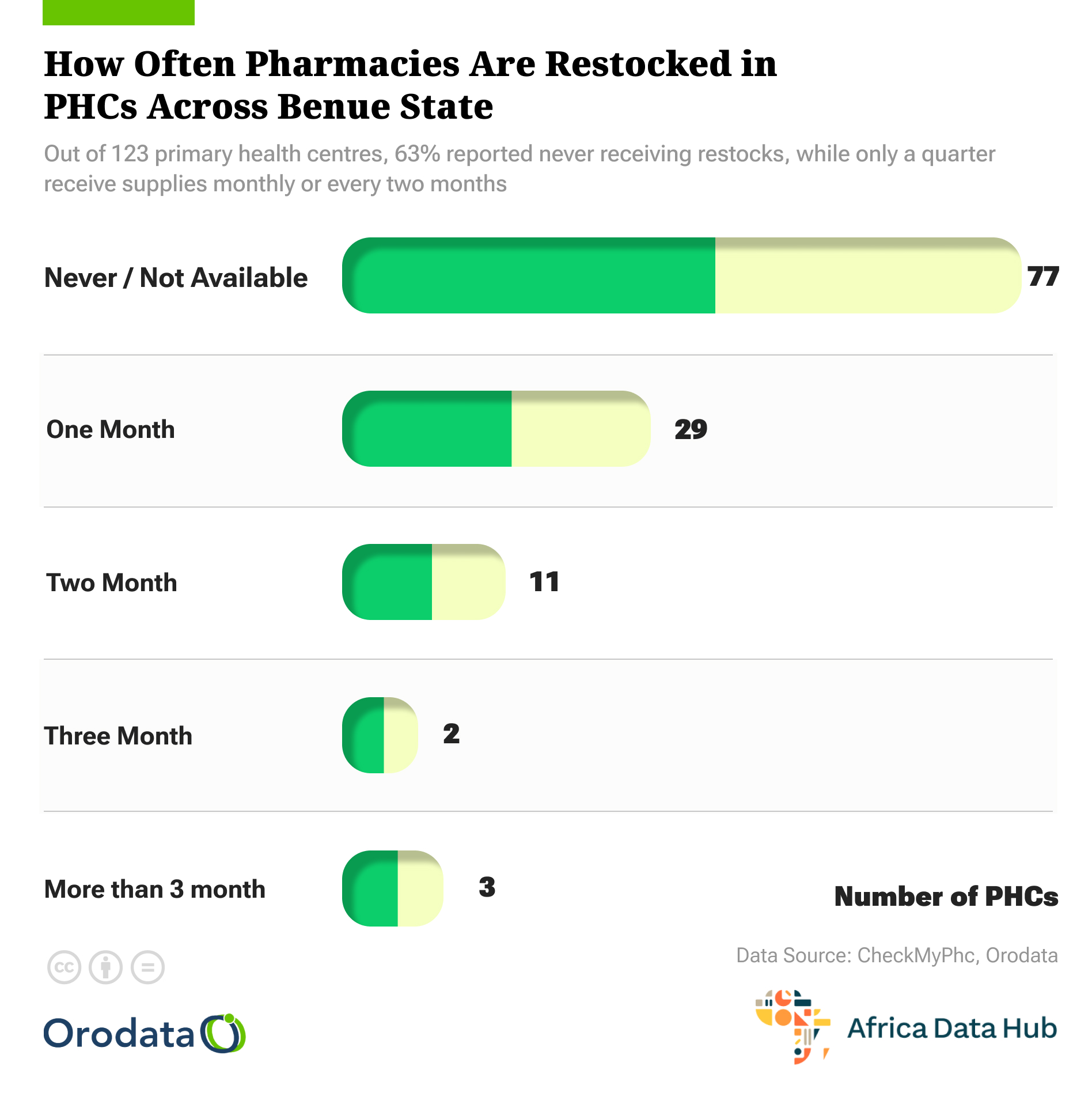
The call went through, but the OIC advised that she be taken to the general hospital at Obarike, the local government headquarters, due to a drug stockout for several months and a lack of beds at the facility.
Unending drug stockouts and the absence of health workers at the primary healthcare centres (PHCs) have consistently widened the health risks of the locals.
Communities Seek Self-Medications Amid Drug Shortages
For years, communities relied on their local PHCs as the first point of care. Now, the stark reality of consistently empty shelves and a lack of essential supplies has created a “new normal” where individuals bypass these crucial facilities entirely.
Elijah was taken to the general hospital but could not be admitted the same day due to lack of bed space. The next day, with much pleading with the nurse, she was offered a bed. Elijah spent a week in the hospital until her recovery.
READ ALSO.
Decades of Bloodshed: How a Lingering Land Dispute Fuels Death, Displacement, and Despair in Benue
ANALYSIS: Crisis in Benue Assembly; How the Suspension of Hon. Blessed Onah Leaves Oju I Constituency in Limbo
Power Outages Cripple Businesses and Healthcare in Benue, Residents Demand Urgent Action
“The sorry state of the PHCs in rural communities is bad, and many locals have turned to seeking alternatives,” Elijah explains.
Her ordeal led to self-medication with antimicrobials anytime feverish symptoms surfaced. “Drug vendors sell similar drugs to what is obtainable at health facilities,” Elijah noted. There are many more with similar experiences, like Elijah unshared.
Onda James, a concerned Okponyire community member, expressed displeasure with the poor infrastructural deficit in government-owned health facilities in Benue State. The health facility is as good as none.
“The lack of basic medicines at the PHCs does not just delay care—it drives dangerous practice of self-medication in the community,” James noted.
Residents Turn to Street Drug Dealers
Two weeks before Christmas, my daughter fell sick. She was taken to the health outpost, but due to a drug stock-out, there wasn’t even a paracetamol to give her, Mary Iji from the Okponyire community recalled. The health worker could only advise him to try a chemist’s store in the next town—miles away and hours too late.
One of the PHCs with Drug shortages. Photo Credit: Okponyire Health Outpost, captured by David Arome
Frequent drug stock-outs at the local health post have pushed residents to take matters into their own hands. With no access to essential medicines, many turn to nearby chemist shops or street vendors, often buying antibiotics without prescriptions.
“Now, once someone falls ill, we just go get drugs ourselves. We can’t wait for the health centre anymore.” Iji admits.
This rising trend of self-medication—especially with antibiotics—is fuelling a quiet crisis. Without proper guidance or diagnosis, people misuse antimicrobials, unknowingly contributing to antimicrobial resistance (AMR), a growing global threat.
READ ALSO.
Decades of Bloodshed: How a Lingering Land Dispute Fuels Death, Displacement, and Despair in Benue
ANALYSIS: Crisis in Benue Assembly; How the Suspension of Hon. Blessed Onah Leaves Oju I Constituency in Limbo
Power Outages Cripple Businesses and Healthcare in Benue, Residents Demand Urgent Action
For Okponyire and communities like it, the lack of basic medicines doesn’t just delay care—it drives dangerous habits that could cost even more lives in the long run.
Access Without Caution
United Nations projections indicate that, by 2050, AMR will account for over 10 million deaths annually, matching the annual death toll of cancer, and US$1 trillion in additional healthcare costs worldwide.
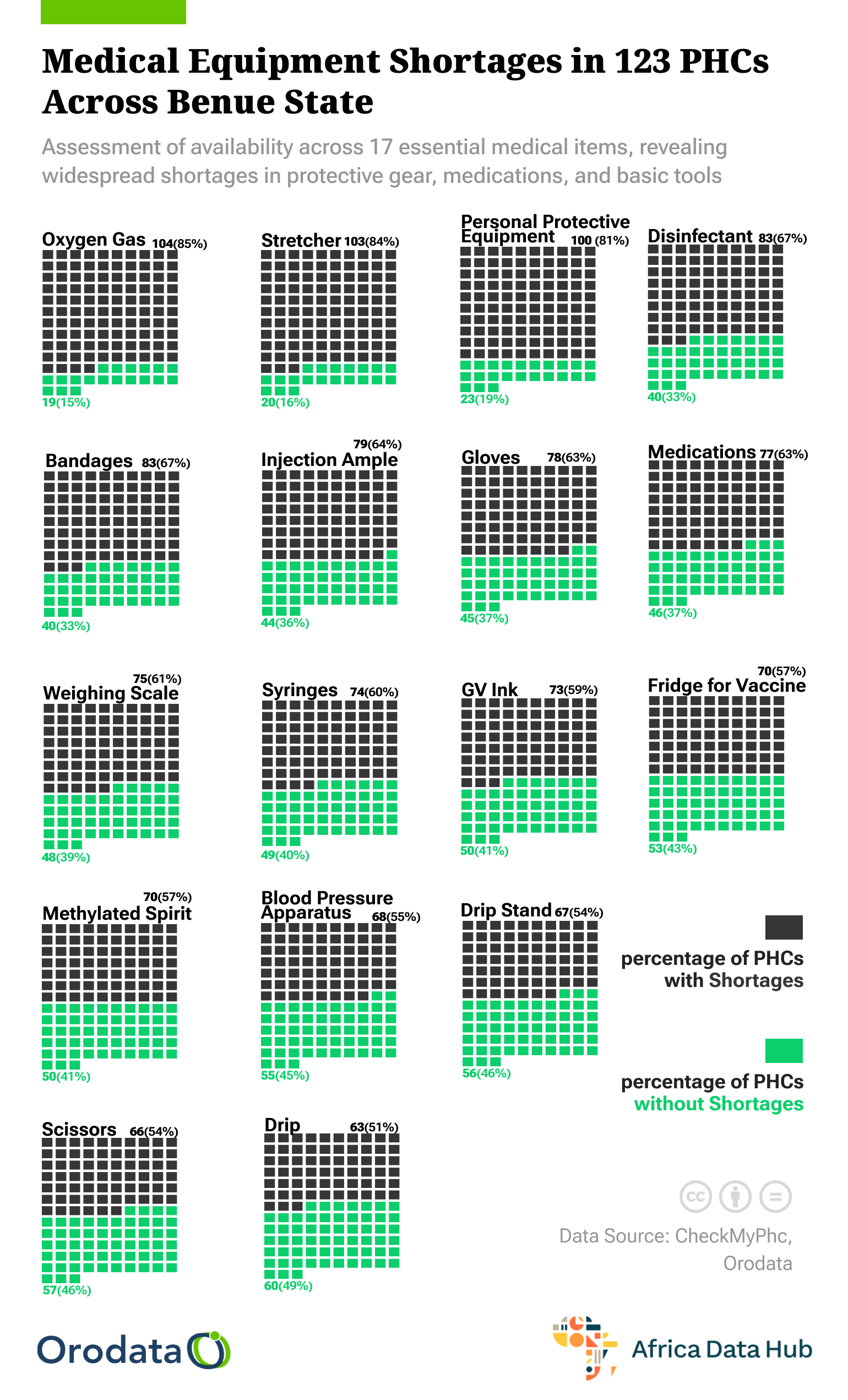
Nigeria is not exempt from this global burden, as AMR knows no boundaries, not even local communities. The increasing self-medication of antimicrobials coupled with poor health infrastructure deficits across the health facilities fuels the AMR rise. It is quite alarming that most government-owned PHCs have been out of drugs, equipment, and health personnel for years. These effects have negated the primary roles of the PHCs to mere prescription rooms. Referring clients to chemist stores and local drug dealers to get drugs. The trends have turned the interest of the locals to self-medication at a “chemist store”
Most of the drugs often misused and overused by the locals are antimicrobials, which they easily get from local drug dealers. Though Nigeria’s National Drug Policy (NDP) classifies antimicrobials as prescription-only medicines, enforcement remains abysmal. The implementation gaps heighten the misuse and overuse of antimicrobials, scaling up AMR.
Drug Shortages; Call for Government Action
Monday, Esim, the officer in charge of the Imadi primary healthcare centre, highlighted the infrastructure deficits, shortages of staff, continued stockouts of drug supplies, and space issues that hinder the facility’s ability to provide quality care. He emphasised the need for the government to prioritise healthcare services in rural communities and establish well-equipped health facilities.
Esim stressed the need for the government to prioritise healthcare service in rural communities. Revamping the ailing healthcare system and putting up fully equipped health facilities for quality healthcare service delivery not just in the Imadi community but also in other settlements in Obi LGA. Esim adds that the ongoing neglect is silently fueling antimicrobial resistance (AMR), as residents increasingly resort to unregulated treatments.
This story was produced for the Frontline Investigative Program and supported by the Africa Data Hub and Orodata Science.